A World Health Organization report warns we’re moving toward a world where antibiotics don’t work
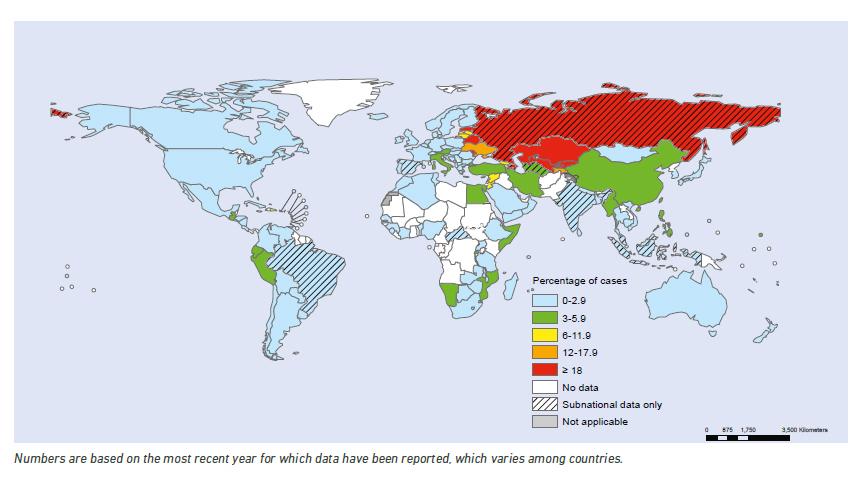
Cases of drug-resistant microbes are on the rise around the world, especially bacteria resistant to antibiotics. This map from the World Health Organization shows the proportion of cases of tuberculosis that are resistant to multiple drugs.
There's a new report out today from the World Health Organization on the spread of drug-resistant microbes, and it's a pretty scary document.
It concludes that the world may be heading into a "post-antibiotic era" in which common infections and minor injuries can kill, essentially returning us to a pre-20th century world in terms of many diseases.
"Far from being an apocalyptic fantasy," the report warns, this is "a very real possibility for the 21st century."
The problem is driven in large part by overuse of antibiotics and other drugs aimed at infectious diseases. It's been growing for years, so the WHO report comes as no surprise to researchers and activists. But Laura Piddock, a professor of microbiology at the University of Birmingham in the UK, says it's the most comprehensive report to date and should be a wake-up call to governments around the world.
"They've gathered together all available information from around the world and shown that the number of antimicrobial-resistant microorganisms is really quite frightening," says Piddock, who's also the director of the group Antibiotic Action.
Piddock says drug-resistant microbes flow "all ways" around the world, from rich countries to poor and vice versa. "So what is someone's problem today will be everyone's problem tomorrow."
"This is evolution in process," she says. "Bacteria grow very quickly … [so] when they're put under pressure to survive, they're going to accumulate mutations that allow them to survive very, very quickly. So if the hostile environment is antibiotic exposure, then these [resistant] bacteria are going to emerge. … And so the more we're exposing bacteria (to antibiotics), the more opportunities for them to become resistant."
The problem has become so extensive and global in nature that Piddock likens it to climate change in terms of both the scale of the problem and the need for a massive, global response. The big difference, she says, is that while "there are people skeptical of the scientific evidence about climate change, there are no skeptics about the evidence about the impact of antibiotic resistant bacteria to human health."
As extensively as the report is able to document the problem, it also makes clear that it is still under-reported, and that far more research is needed to track and understand the problem.
Piddock agrees with that prescription, but points to two other big changes that are needed to grapple with the threat.
"The easiest way we can start tackling this is to minimize antibiotic use in all settings, whether it is a doctor, a veteranarian, a food producer or indeed ourselves in the home," she says. "The less we expose bacteria to antibiotics, the less chance they have to become resistant. So we've all got a part to play in this."
And she says there's an urgent need for new drug development.
"The [drug] pipeline has got very, very slow and is not really being populated very much. So we need a lot more basic research, and a lot more discovery and development," she says.
There's a new report out today from the World Health Organization on the spread of drug-resistant microbes, and it's a pretty scary document.
It concludes that the world may be heading into a "post-antibiotic era" in which common infections and minor injuries can kill, essentially returning us to a pre-20th century world in terms of many diseases.
"Far from being an apocalyptic fantasy," the report warns, this is "a very real possibility for the 21st century."
The problem is driven in large part by overuse of antibiotics and other drugs aimed at infectious diseases. It's been growing for years, so the WHO report comes as no surprise to researchers and activists. But Laura Piddock, a professor of microbiology at the University of Birmingham in the UK, says it's the most comprehensive report to date and should be a wake-up call to governments around the world.
"They've gathered together all available information from around the world and shown that the number of antimicrobial-resistant microorganisms is really quite frightening," says Piddock, who's also the director of the group Antibiotic Action.
Piddock says drug-resistant microbes flow "all ways" around the world, from rich countries to poor and vice versa. "So what is someone's problem today will be everyone's problem tomorrow."
"This is evolution in process," she says. "Bacteria grow very quickly … [so] when they're put under pressure to survive, they're going to accumulate mutations that allow them to survive very, very quickly. So if the hostile environment is antibiotic exposure, then these [resistant] bacteria are going to emerge. … And so the more we're exposing bacteria (to antibiotics), the more opportunities for them to become resistant."
The problem has become so extensive and global in nature that Piddock likens it to climate change in terms of both the scale of the problem and the need for a massive, global response. The big difference, she says, is that while "there are people skeptical of the scientific evidence about climate change, there are no skeptics about the evidence about the impact of antibiotic resistant bacteria to human health."
As extensively as the report is able to document the problem, it also makes clear that it is still under-reported, and that far more research is needed to track and understand the problem.
Piddock agrees with that prescription, but points to two other big changes that are needed to grapple with the threat.
"The easiest way we can start tackling this is to minimize antibiotic use in all settings, whether it is a doctor, a veteranarian, a food producer or indeed ourselves in the home," she says. "The less we expose bacteria to antibiotics, the less chance they have to become resistant. So we've all got a part to play in this."
And she says there's an urgent need for new drug development.
"The [drug] pipeline has got very, very slow and is not really being populated very much. So we need a lot more basic research, and a lot more discovery and development," she says.