Antibiotic use fuels drug resistant superbugs from India
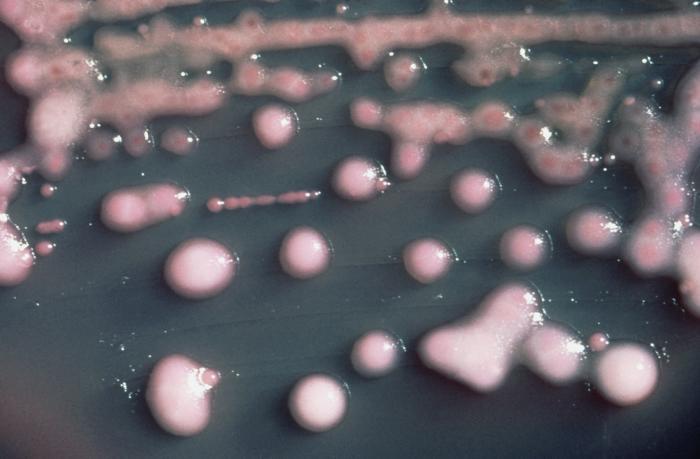
A story in the latest issue of Bloomberg Markets Magazine portrays India as a veritable breeding ground for drug resistant germs that now threaten the world.(Photo courtesy of the Public Health Image Library via the CDC.)
The antibiotics that have saved countless lives since the discovery of penicillin in the 1920s have a problem: Many germs are developing immunity to those life-savers.
Drug resistance can spread like wildfire when bacteria of various kinds exchange genetic material. This is exactly what has happened in the last century — because of overuse and improper use of antibiotics. It’s a global problem, but one country — India — may play an outsized role in fueling it.
Health reporter Jason Gale, whose story on the topic appears in the June issue of Bloomberg Markets Magazine, said India’s booming generic drug industry, which has fostered the widespread overuse of antibiotics, is causing bacteria to develop resistance to drugs.
“The thing about India which makes it unique, I think, is that when you look at the drivers of drug resistance, India pretty much ticks every single box,” Gale said.
In addition, Gale said, India’s poor sanitation and lack of toilets allows germs to spread easily from people, into the environment and back to people. India’s role as a medical tourism hub means people worldwide may be exposed to resistant germs.
In India, one gene in particular has spread to many bacteria, making them resistant to antibiotics. Scientists named this gene NDM-1 for New Delhi — the city where it was discovered and the enzyme the gene produces. The gene was found in a Swedish man of Indian origin in 2007. Swedish doctors cultured bacteria from him and discovered that it resisted most antibiotics.
Some Indian politicians are worried that the discovery of these drug-resistant bacteria could tarnish India’s reputation as a destination for medical tourism.
“There’s quite a bit at stake. The country is definitely wanting to be a medical tourism hub and is very keen to protect that industry,” Gale said.
Though the very modern hospitals work hard to keep these drug-resistant germs out, Gale said they aren’t immune from the risk.
“Doctors and nurses, and food, they’re all coming in from outside and unfortunately the outside does carry this risk,” he said. “With this NDM-1 gene, it really only leaves two or three antibiotics that could potentially treat bacterial infections.”
But India isn’t the only source of these lethal bacteria. They are present all over the world. In countries like the United States, agriculture is the biggest user of antibiotics. Low doses of antibiotics work as a growth promoter in animals, which reduces costs for farmers.
According to an investigation in the Washington Post, of the 35 million pounds of antibiotic used in the US in 2008, 70 percent “went to pigs, chickens and cows.” Worldwide, that number is about 50 percent.
For decades, scientists have documented how antibiotic resistance can evolve on farms and spread to people. As early as 1976, Stuart Levy of Tufts University showed that highly drug resistant E. coli on farms can pass easily to farm workers in a matter of a few weeks.
A study published earlier this year in the journal mBio, illustrated how these drug-resistant bacteria are spreading around the globe.
The study involved a recently evolved strain of MRSA called CC398. For about a decade, this strain has been spreading through poultry and pig farms around the world, and has also infected many people.
Lance Price of the Translational Genomics Research Institute in Phoenix and his team of researchers discovered that the organism started off as a methicillin sensitive bacterium in humans. Once it jumped to farm animals, it rapidly evolved resistance and did so multiple times on multiple farms. The new drug resistant form, called livestock-acquired MRSA then jumped back to farm workers.
“It’s no big surprise that we’re seeing this,” Price said. “I’m sure we’re going to see this multiple times in the future, if we’re going to continue to use antibiotics in these filthy CAFOs (Concentrated Animal Feeding Operations).”
Several countries, including the United States, are trying to reduce antibiotic use on farms with varying effects.
Sweden was the first country to ban the use of antibiotics as growth promoters. Since then, Denmark, the Netherlands followed suit and, most recently, the European Union restricted the use of antibiotics on farms. The FDA also announced a rule that will require farmers to have prescriptions in order to use antibiotics.
These bacteria and their genes are spreading so rapidly around the world that some scientists regard the resistance genes as a new kind of environmental contaminant. The World Health Organization described the problem as the beginning of a potential post-antibiotic era.
“We are coming to the end of the road when it comes to antibiotics and what’s going to be efficacious in many instances,” Gale said.
Our coverage reaches millions each week, but only a small fraction of listeners contribute to sustain our program. We still need 224 more people to donate $100 or $10/monthly to unlock our $67,000 match. Will you help us get there today?