Blood-forming stem cells likely hold the key to curing many types of disease
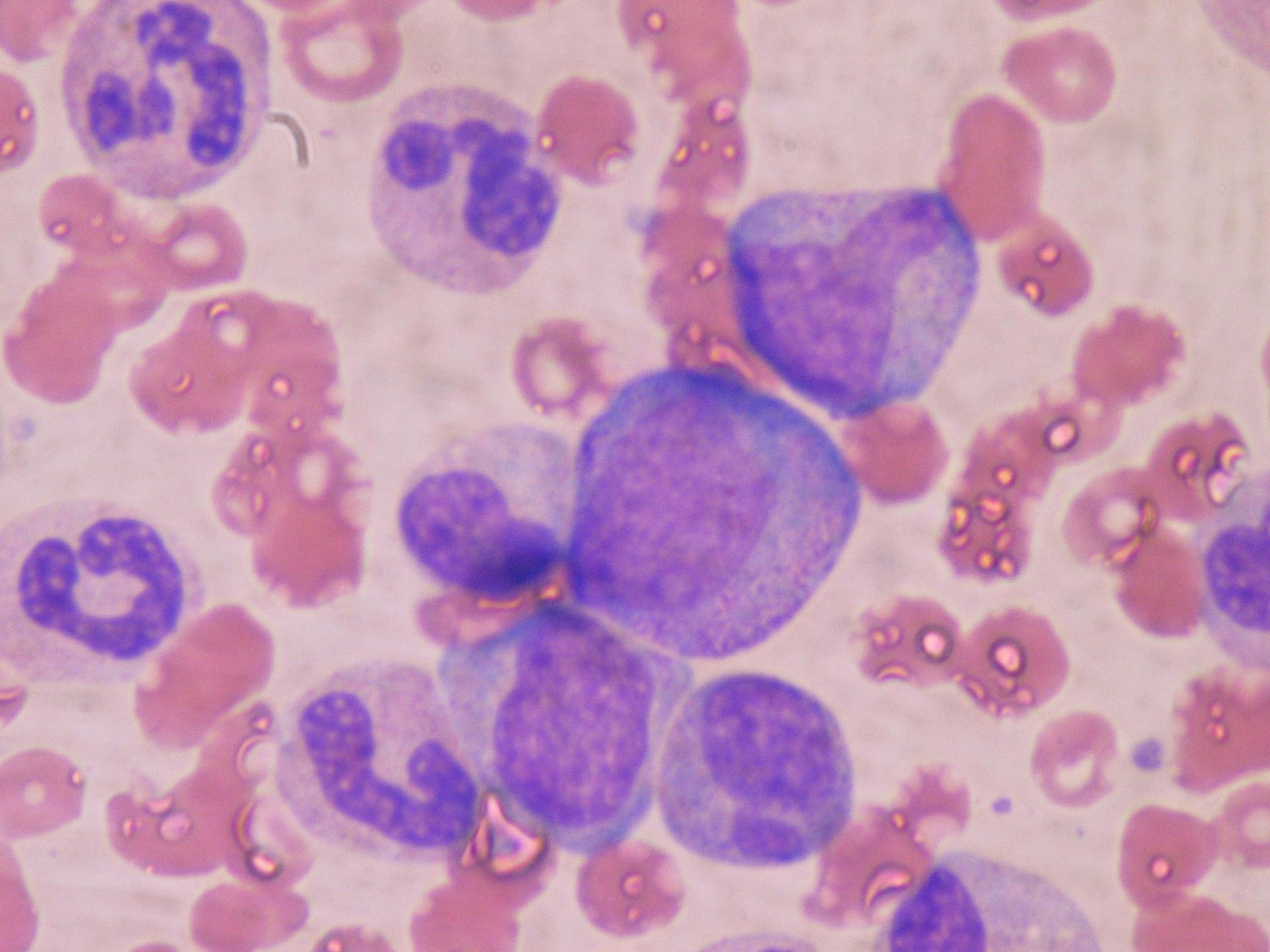
Hematopoietic blood cells — also known as blood-forming cells — have been central to bone marrow transplants for over fifty years. New ways of using these cells may prove beneficial to treating disease.
Researchers at Stanford are reviving a technique that can use uncontaminated, blood-forming stem cells to treat a patient with cancer, autoimmune deficiency and other diseases.
Beginning in the 1960s, hematopoietic, or blood-forming, stem cells became the basis for bone marrow transplants used to treat cancer patients. Then, in the 1980s and 1990s, scientists found a way to stimulate these stem cells to move from the bone marrow into the bloodstream for collection — a process called mobilization — which gradually lessened the need for bone marrow transplants.
According to a 1996 study, the use of mobilized blood cells in cancer patients had multiple benefits: It led to “lower morbidity, and greater cost-effectiveness compared with conventional bone marrow transplant …and the relative ease of obtaining large amounts of stem cells made multi-cycle transplantation a viable option in the treatment of malignancies, allowing further escalation of chemotherapy dose intensity.”
In 1988, Irv Weissman, a longtime stem cell researcher, developed a process that could create "purified" blood-forming stem cells from mobilized blood — that is, they could extract pure, uncomtaminated stem cells from all the other cells in the mobilized blood.
This discovery became important, Weissman says, because of results found in a 1990 trial that treated women with metasticized breast cancer — cancer that has moved beyond the breast and the lymph nodes to the bones, the lung and the liver. These patients had no hope of any localized therapy to save them, but “you could give high-dose chemotherapy, and the more chemotherapy you gave the more cancer cells in the body you killed,” Weissman explains.
“[But] when we looked at the mobilized blood from those women, we saw that over half of the samples [still] had breast cancer cells in them,” he continues. “When we purified the blood-forming stem cell from the [full] mobilized blood, for the first time in medical history we could give back to those women cancer-free stem cells to regenerate their blood-forming system at doses of chemotherapy that, without return of cells, would kill them.”
The company Weissman formed after these clinical trials was bought by a larger company, which shut down the studies on purified blood cells. It is a complicated story, Weissman says, but the long and the short of it is: “They didn't want to go into this research. There’s no money to be made in this sort of thing … They told me it was a business decision.”
Five years ago, Weissman and two other colleagues, retrieved the old data and found that one-third of the women who had received the cancer-free stem cells in the 1996 trial were alive, apparently without disease. Only 7 percent of the women who were treated with full mobilized blood — that is, cancer-contaminated blood — were alive.
Weissman had to give away any financial profit arising from his old company, but now all the materials are back at Stanford, where Weissman is the director of the Institute of Stem Cell Biology in Regenerative Medicine. Thanks to California’s Proposition 71, which created the California Institute of Regenerative Medicine in 2004 and granted power to the state to fund stem cell research independent of any profit-making enterprise, Weissman will have sufficient funds to begin this summer a trial of transplants using purified stem cells.
The first transplants won't be for breast cancer patients right away, he says. He and his colleagues will focus first on patients with blood disorders — diseases like sickle cell anemia, Thalassemia or juvenile diabetes, in which the blood-forming system has genetically gone wrong. In these cases, Weissman says, they can give back purified blood-forming stem cells from a related donor who doesn't have the disease, effectively replacing the defective blood system with one that isn’t defective.
Weissman also plans to approach children with SCID (Sever Combined Immunodeficiency) — a disease in which no adult immune system develops — and transplant these patients with pure, blood-forming stem cells, either from their mother or from a sibling.
“With pure stem cells, we show in animal model after animal model, that we could have a platform for regenerative medicine,” Weissman says. “If you need a lung, you would get a blood-forming stem cell from the lung donor, along with the lung itself, and eventually a lung stem cell. This is the basis for regenerative medicine.”
Two other recent discoveries could advance the field even more, Weissman says.
The discovery of the Crispr enzyme, which can actually edit genetic code, could lead to an even better way to treat a child with SCID. Doctors could use the Crispr enzyme to remove the defective gene and replace it with a healthy gene, so patients get back their own blood-forming stem cells.
Pluripotent stem cell lines, “master” cells that can potentially produce any cell or tissue the body needs to repair itself, also show great promise. “We are working right now on the project, as are many other labs, to get every tissue-specific stem cell from these pluripotent stem cell lines,” Weissman says.
This article is based on an interview that aired on PRI's Science Friday with Ira Flatow