Some major news today in the fight against the coronavirus: President-elect Joe Biden said he’ll release all the doses of the vaccine in the United States when he takes office.
It’s a strategy with some risk: The vaccines from Pfizer and Moderna were designed for two doses. But with so much of the supply currently unused, Biden is essentially betting that with his plan, the country can get morepeople vaccinated and have enough to go around for a second dose.
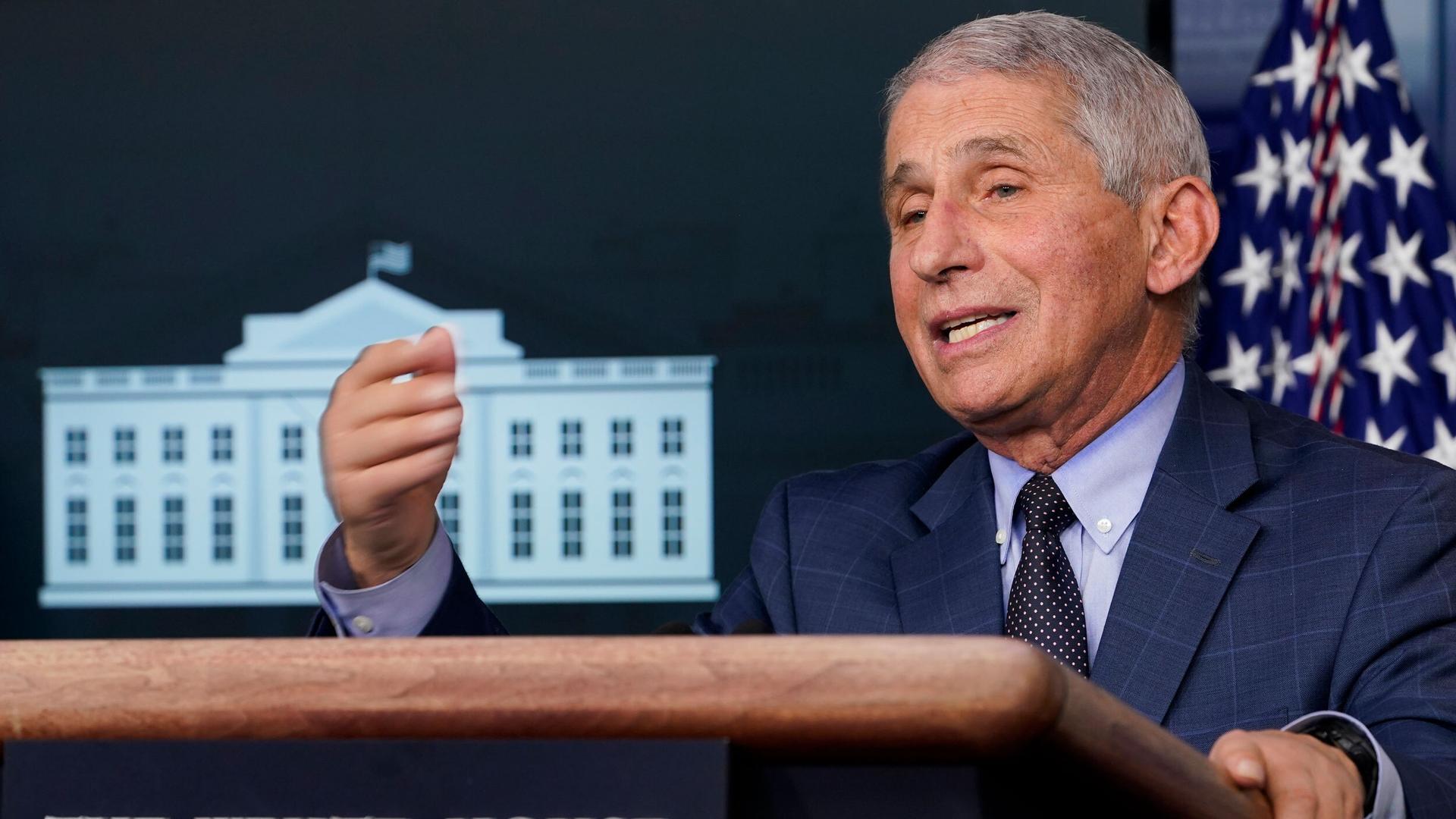
Biden’s decision comes a day after another grim milestone of more than 4,000 COVID-19-related deaths in the US in a single 24-hour period. The US death toll for the entire pandemic has surpassed 365,400. And the nation’s top infectious disease expert, Dr. Anthony Fauci, warns the next few weeks are only going to get tougher.
Fauci will be part of the Biden administration team in charge of managing the pandemic. He spoke to The World’s host Carol Hills about how he sees a way forward to manage the pandemic and why it’s so hard to get politicians and citizens to take it seriously.
Related: The key to overcoming vaccine hesitancy? Deep listening, tailored messaging.
Carol Hills: Dr. Fauci, you’re scrupulous about staying out of politics, but we’ve all observed how our broken politics have stunted the US’ ability to control the coronavirus. How do you, a public health official, see a way forward to manage the pandemic when we cannot get citizens to really understand the problem?
Dr. Anthony Fauci: Well, you know, there’s politics, but there’s also divisiveness in society. That’s something that’s going to take a while to correct. Obviously, we’ve got to keep politics out of public health measures. There’s no place for that. They do nothing but interfere.
But we have a lot of work ahead of us to get the country together and pulling together in an effort to end this outbreak and just put aside things like the politicization of wearing of masks and doing other public health measures.
WHO director Tedros Ghebreyesus said this week that the world “has entered a new phase of the pandemic where solidarity is needed like never before,” that we’re in a race to save lives right now. What does that mean to you and how do you assess this period we’re in?
I think we were in this period all along. Whenever you have a global pandemic, you have to have solidarity between countries because what affects one country in one part of the world, when you’re dealing with a communicable disease that has a high degree of efficiency and transmitting from person to person, you have to have interconnectedness with regard to cooperation, collaboration and solidarity, because viruses, particularly viruses like SARS-CoV-2 that are spectacularly efficient in their ability to transmit, they don’t know borders at all. So, since they don’t know borders, we sort of have to act like we don’t know borders and we’re all in this together.
Related: An immunologist answers three questions about the COVID-19 vaccine
Can we vaccinate our way out of this pandemic?
The answer is yes — just the way we have vaccinated our way out of multiple public health threats such as smallpox, polio, measles and a number of others. So when you’re dealing with communicable diseases, infectious diseases, very often the gold standard of how to really crush these outbreaks is by getting a safe and highly efficacious vaccine. We are very fortunate in that we already have two and likely we’ll have more than that — vaccines with a very high degree of efficacy. The Moderna and the Pfizer products are 94-95% efficacious.
So if we get, and I’ve made an estimate, it’s purely an estimate, about 70-85% of the population vaccinated, I believe we would have what’s called an umbrella or a blanket of herd immunity over the country. And if the rest of the world does that, we could crush this outbreak. Absolutely. Vaccine is the answer. Until we get a vaccine, we must concentrate very, very clearly on the public health measures that we talk about all the time: namely, uniform wearing of masks, keeping physical distancing, avoiding crowds in congregate settings, particularly indoors and washing your hands frequently. That should be the bridge to the vaccine. But if we can get the overwhelming majority of people vaccinated, we can put an end to this outbreak.
The vaccine rollout in the US has been off to a slow start in so many areas. What do you see as being the biggest holdup?
Well, I think there are a number of things that are going on. Right now, we are still in the very early stages. Whenever you introduce a massive program, the likes of which we’ve not had before, namely vaccinating essentially all of the country or the overwhelming majority of the country with a brand-new vaccine program, that, not surprisingly, can get off with some bumps in the road and some hiccups. Having said that, that’s not an excuse. We’ve got to do better. We must do better. What I’m saying is that let’s give it a week or so into January to see if the process can catch up with the pace that had originally been put forth.
Another key feature of the US health system is this kind of state-level versus federal and then local. And in terms of vaccine delivery, the Trump administration has left it up to the states to sort out the vaccine delivery. Is that the right way to proceed? And do you see that changing under a Biden administration?
Yes, no doubt it’s going to change because in the discussions that I’ve had in my new role of being part of the COVID[-19] team and the general public health team of the Biden group, is that we will have a much more close interaction between the federal and the state level in the sense of planning together, as well as implementation and support.
Right now, the issue that is confronting us is that we need to more efficiently get vaccines into the arms of people. We have more vaccine distributed than we’ve actually put into the arms of individuals. We need to do better with the doses we have.
When it comes to who gets a vaccine, in Nebraska, the governor initially said that undocumented immigrants would not be included in plans to vaccinate workers at meatpacking plants. What are the repercussions of bringing immigration status into vaccine eligibility and priority?
From a public health repercussion, you got to get people vaccinated. It doesn’t matter who they are. If you’re in the country, you’re a threat of getting infected yourself and of transmitting the infection. So there’s no room for any withholding of vaccines for people because they’re part of the population that we’re dealing with.
Do you see any successful models from elsewhere in the world that the US could emulate?
Well, I don’t think so, because no one has yet gotten into this in a really large, meaningful way. This is really quite unprecedented. There have been situations that — if you go historically, not as an example of what other countries are doing, because each country is different, depending upon the size and the health system…for example, those countries that have national health services where everything is interconnected, it can generally be much easier to implement something like this. But if you go back in history and look at times when we’ve had to do mass vaccination programs, there likely could be some lessons learned there.
There is a very interesting historical story about that. In 1947, we had someone visit Mexico as a tourist and then come back to the United States having contracted smallpox in Mexico — came back to New York City, and actually infected a bunch of people. They were 12 hospitalizations and two deaths. New York City, in response to that, did a massive vaccination program. And in a three-week period, they vaccinated 6,350,000. And within two weeks, they vaccinated 5 million people just in New York City. Of note, I was a 6-year-old boy who was one of those 6,350,000 people that were vaccinated in New York. So, if New York City can vaccinate 6,350,000 people in three weeks, and that’s only one city, then we can go back and get some lessons learned, how that was done, and get it done country-wise.
This interview has been edited and condensed for clarity.
Our coverage reaches millions each week, but only a small fraction of listeners contribute to sustain our program. We still need 224 more people to donate $100 or $10/monthly to unlock our $67,000 match. Will you help us get there today?