New treatments, new hope for opioid epidemic
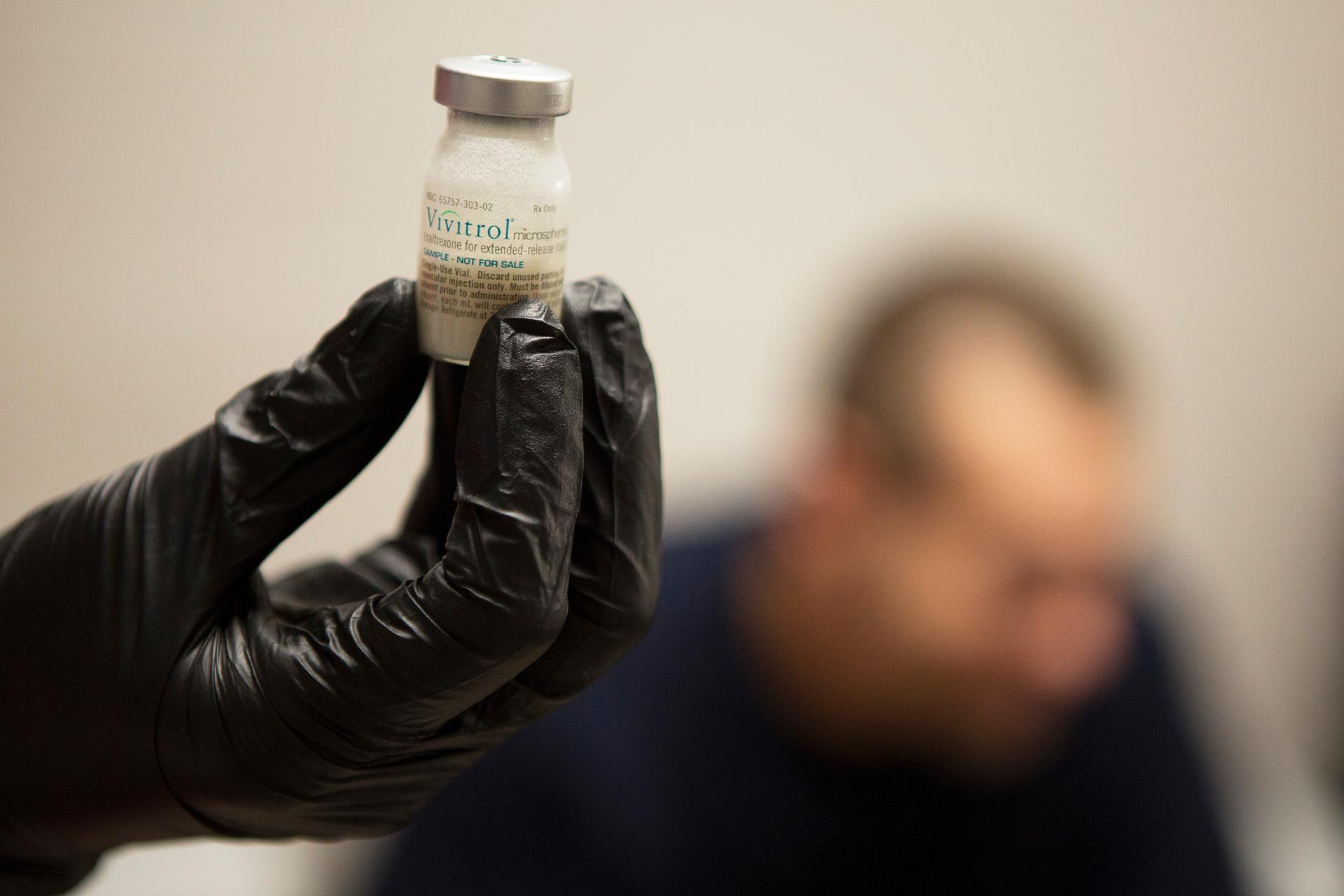
Gail Dufault, the Transitional Healthcare Coordinator at the Barnstable County House of Corrections, checks that a dose of Vivitrol is mixed properly before administering the drug to inmate Kenneth Saglibene at the prison in Buzzards Bay, Massachusetts September 2, 2014. Barnstable is believed to be the first jail in the country to launch an intensive voluntary recovery program for opiate-addicted inmates with the use of Vivitrol, an injectable non-narcotic drug that blocks receptors in the brain and bars addicts from getting high off heroin and other opioids for about 25 days, at a cost of about $1,000 a shot.
In the past two decades, the devastation associated with opioid addiction has escaped the relative confines of the inner city and extended to suburban and rural America. Due in large part to the proliferation of prescription pain relievers, rates of opioid abuse, addiction, overdose and related deaths have increased dramatically. This has affected families and communities that once felt immune to this crisis.
On Aug. 1, an analysis of health care claims for treatment of opioid dependence showed a 3,000 percent increase from 2007 to 2014.
The knowledge that many are afflicted or affected has helped people understand the powerful psychological and physiological grip of addiction. As a result, stigma has decreased.
What was once relegated to the back burner of public concern has become a top public health priority.
We addiction experts also have gained better understanding of the illness, and we see reasons for hope.
Shifts in public policy
The Affordable Care Act and the Mental Health Parity and Addiction Equity Act combined to finally require insurance companies to cover treatment for patients suffering from addiction. Insurance companies can no longer deny treatment or significantly limit treatment for psychiatric disorders, including addiction, as they had in the past.
President Obama recently proposed $1.1 billion in funding to expand access to treatment for opioid addiction and overdose prevention.
In July, the House passed a bill that would further expand access to care for addiction and other mental health conditions.
Then, on July 22, the president signed into law the Comprehensive Addiction and Recovery Act of 2016.
If adequately funded by Congress, the law will help to strengthen prevention, treatment and recovery efforts.
This improves treatment options for individuals in the criminal justice system, which may decrease rates of return to crime and prison. It also expands access to naloxone, a lifesaving drug that emergency medical workers and even family and friends, in certain cases, can administer to someone who has overdosed.
This stepped-up policy response is giving doctors the means to better treat people with opioid addiction. When combined with improvements in public understanding that addiction is a disease requiring treatment, we as a society are creating an environment that supports treatment. We believe this will save many thousands of lives.
A societal effort
Physicians are re-examining their own prescribing practices to decrease the likelihood of medication diversion or misuse and to minimize the development of iatrogenic addiction, or addiction that stems from medical treatment.
Law enforcement officials have worked to close down hundreds of “pill mills,” or clinics purporting to serve patients with chronic pain disorders. In reality, they serve as primary access points for dealers selling prescription drugs on the black market.
In all states except Missouri, prescription drug monitoring programs have also helped to identify patients in need of intervention.
More patients have access to treatment than ever before, including many in the criminal justice system who participate in drug court diversionary programs. Such programs save taxpayer money and decrease recidivism.
Greater understanding and knowledge
The field of addiction medicine has matured and expanded, recently acquiring recognition as a dedicated medical specialty.
According to the American Society of Addiction Medicine, the disease of addiction is best understood as a single condition. There is no distinction made depending on the preferred drug(s) of abuse.
Addiction specialists conceptualize addiction as a bio-psycho-social-spiritual disease. They understand that continued use of psychoactive substances interferes with active participation in psychosocial treatment. Such usage prevents development of a personal program of recovery.
Therefore, successful treatment of opioid addiction begins with abstinence from all substances of abuse. Patients should not expect to quit using oxycodone, fentanyl or heroin but continue to drink alcohol or to smoke marijuana. The same holds true for treatment of addiction to alcohol, marijuana, cocaine or any other drug.
Some patients require medically supervised detoxification to abstain. Accessing the right treatment is crucial to success. Some will need a more intensive treatment setting. Even individuals who were unsuccessful maintaining abstinence with outpatient treatment may achieve recovery in a more intensive treatment setting.
Addiction, like other medical conditions with significant behavioral components, is a chronic condition. Relapse may occur. Thus, most patients need to learn skills that help them cope adaptively with stressors in their daily lives. Often, they need to address issues from their past that relate to substance abuse.
People with addiction may have other psychiatric conditions. They need to be treated for those, too. In many areas, publicly funded treatment programs are available for individuals lacking insurance or who cannot afford private treatment.
Support from family and 12-step programs helpful
Family members should encourage patients suffering from addiction to seek a professional evaluation. This will help determine the appropriate level of care, which could range from outpatient management to long-term residential treatment.
In addition, physicians and other treatment specialists highly encourage participation in a 12-step recovery program, such as Alcoholics Anonymous or Narcotics Anonymous. Such programs are free, and they offer many benefits. Research has documented significantly reduced risk of relapse with increased likelihood of successful outcome among patients treated for opioid addiction in this way.
Family members often benefit from 12-step programs, too. Al-Anon or Alateen can help them learn how best to support their loved one without enabling the addiction.
Medications also helpful
Patients with opioid use disorders may also benefit from medication assistance. Currently, four types of prescription medication are approved to assist with treatment of opioid addiction.
The opioid antagonist medication, naltrexone, is available as a daily oral pill or as a monthly intramuscular injection. It helps patients by decreasing cravings. It also blocks patients' ability to “get high,” even if they use an opioid drug. Naltrexone has no abuse potential, and can be safely used by most patients.
Second, the opioid partial agonist medication buprenorphine is available as an oral pill, dissolving tablet or filmstrip. It also reduces cravings and reduces and prevents withdrawal symptoms. It, too, blocks the ability to “get high.”
Buprenorphine has some abuse potential, however. It should be used only under guidance and careful monitoring by a physician with sufficient expertise. In fact, doctors must receive a waiver to be allowed to prescribe buprenorphine.
Third, the opioid agonist medication methadone prevents withdrawal symptoms, reduces cravings and interferes with the ability to “get high” from other opioids.
Methadone also has abuse potential and risk of overdose if used inappropriately, however. As a result, methadone is typically dispensed in liquid form on a daily basis, and only from specialized methadone maintenance treatment clinics.
Finally, for individuals at high risk of relapse, new measures are in place to help prevent death in the event of accidental overdose. The opioid antagonist medication naloxone is now available in an automatic injector formulation for use by police, EMTs and other first responders. Naloxone has long been used by medical professionals in emergency rooms to reverse opioid overdose.
Naloxone is also available by prescription for patients with opioid addiction and their families to keep on hand as a safety precaution. In some states it is also available over the counter at certain pharmacies. It can be viewed much like an Epi-pen, which patients with severe allergies keep on hand for emergencies. A naloxone nasal spray is newly available, which may further facilitate access to this lifesaving medication.
These changes to public policy and advances in opioid treatment have greatly improved the prognosis for patients suffering from opioid addiction. Research and clinical evidence have demonstrated that long-term recovery is not only possible, but expected, following adequate treatment with appropriate follow-up care.
Now, more than ever, there is hope for healing from addiction.
![]()
William Greene, Assistant Professor, Psychiatry, University of Florida and Lisa J. Merlo, Associate Professor, Psychiatry, University of Florida
This article was originally published on The Conversation. Read the original article.
The story you just read is accessible and free to all because thousands of listeners and readers contribute to our nonprofit newsroom. We go deep to bring you the human-centered international reporting that you know you can trust. To do this work and to do it well, we rely on the support of our listeners. If you appreciated our coverage this year, if there was a story that made you pause or a song that moved you, would you consider making a gift to sustain our work through 2024 and beyond?