In Ebola response, Big Pharma and public sector strive to make up for lost time
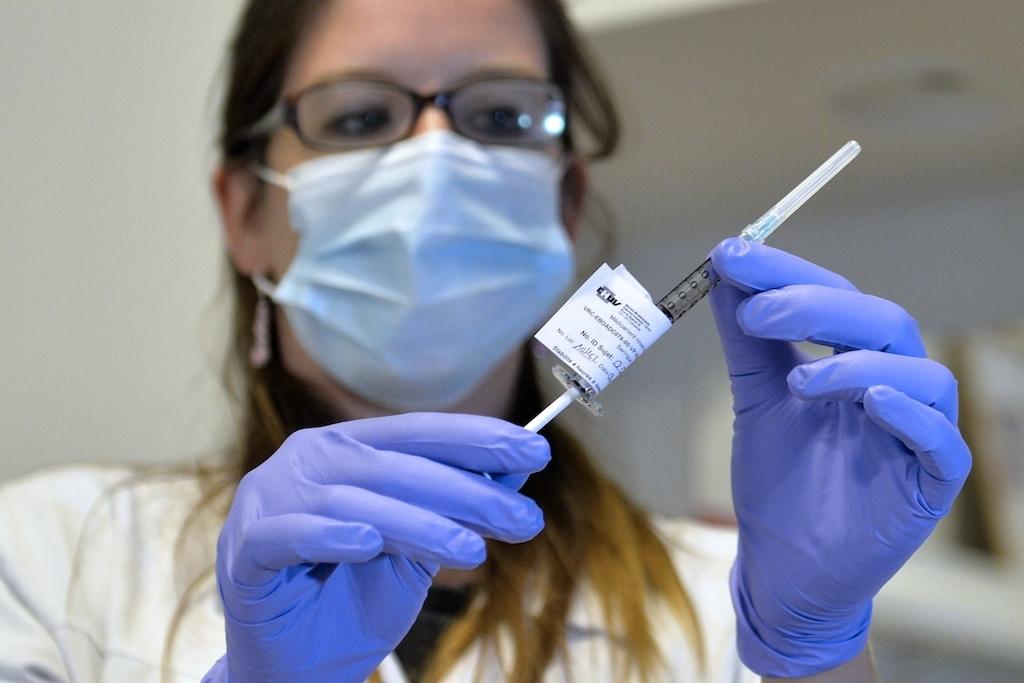
A doctor holds a syringe containing the Ebola vaccine made by Britain’s GlaxoSmithKine during trials on November 4, 2014 at the CHUV hospital in Lausanne, Switzerland.
By the time the first Ebola cases were diagnosed in the United States and Europe early last fall, the deadly, destructive disease had already killed thousands of people across five countries in West Africa.
Only then, with fears of a global epidemic spreading even more quickly than Ebola itself, did private pharmaceutical companies begin teaming up with government entities to move forward with developing an Ebola vaccine. The delayed response is an example of the diverging interests of public and private sectors when it comes to addressing a public health crisis, say experts from both sides.
A new law passed by the US Congress last month aims to close this gap, providing government subsidies to private companies in order to expedite the development of an Ebola vaccine. Under the law, the handful of pharmaceutical companies currently racing to produce viable vaccine candidates could get their candidates to market within six months of finishing clinical trials.
At a public lecture at Georgetown University this week, World Bank President Jim Yong Kim underscored the importance of public-private partnerships for responding to a health epidemic like Ebola.
"The private sector does have a huge stake in helping us,” he said. “We need to get the people who are never in rooms together, to sit together. We have got to make sure that these conversations happen.”
Still, some experts question whether the public-private partnership model will be successful in making a vaccine available to the poorest populations. They caution that when private companies get involved in public health, profit motives could dictate who ultimately benefits from the drugs.
“The [law] creates incentive for the private sector and doesn’t ask anything in exchange,” says Judit Rius, the access campaign manager of Doctors Without Borders/Medecins Sans Frontieres (MSF). “That’s a failure.”
A subsidy for private vaccine development
The science and technology to produce an Ebola vaccine have existed for decades, experts say, but private companies never invested much in the effort because there was no profit to be made.
“The development of an Ebola vaccine was languishing because of a lack of a sustainable commercial market,” says Aurélia Nguyen, director of policy and market shaping at the GAVI Alliance, an international organization that purchases over a billion dollars worth of vaccines annually to inoculate the world’s poorest communities.
The new legislation passed in December adds Ebola to an 8-year-old Food and Drug Administration program that incentivizes companies to develop drugs for neglected tropical diseases.
Under the Priority Review Voucher (PRV) program, first authorized by Congress in 2007, pharmaceutical companies can purchase vouchers for an expedited FDA review and get products on the market within six months of completed clinical trials. Although each voucher’s cost — as much as $10 million — is significant for the pharmaceutical companies, the benefit of getting drugs to the market faster often outweighs it.
The vouchers are potentially worth hundreds of millions of dollars and can be sold between companies. Last November, a PRV for the parasitic disease leishmaniasis was sold by Knight Therapeutics to Gilead Sciences for $125 million.
Proponents of the new law believe the vouchers will get the much-needed vaccines onto the market faster.
“[Ebola] is the closest thing we have to smallpox,” says CDC spokesman Frank Mahoney.“We have to get this back in the box or we’re going to be plagued by it.”
Other experts criticize the law because for-profit companies stand to benefit from large public subsidies, yet they are not required to provide their products at an affordable cost to countries that need it most. For example, under the bill, a pharmaceutical company would be able to patent its vaccine. But it would not be required to share its research with other companies or research institutions – a lack of transparency that could hinder the drug’s availability and affordability.
MSF’s Rius considers the new law a missed opportunity to require the resulting treatments and vaccines to be considered public goods, accessible to those who need them.
“Society might end up paying twice,” she says, “as a taxpayer at the beginning and then again as a consumer.”
Vaccines in the pipeline
Several private companies are working with the public sector in public-private partnerships (PPPs) to produce an Ebola vaccine. Their efforts make them eligible for the PRV to prevent Ebola. One frontrunner in clinical trials is led by GlaxoSmithKline and the US National Institute of Allergy and Infectious Diseases (NIAID).
Although NIAID began testing three Ebola vaccine candidates in 2003, the vaccines were never developed because there wasn’t enough of a commercial incentive for companies keeping an eye on their profit margins.
“Getting a company to invest in an Ebola vaccine instead of something else is difficult,” explains MSF’s director of policy, Rohit Malpani. “The costs are very high compared to developing other vaccines that are blockbusters and make a lot of money.”
GSK joined NIAID’s effort in 2013, after having acquired a Swiss biotech company that had been working on an Ebola vaccine for a few years, but didn’t launch clinical trials on humans until September 2014, well into the current West African outbreak.
The delay in getting vaccine trials underway, says GSK spokesperson Mary Rhyne, was a result of the fact that Ebola “was not on anyone’s priority list… Nobody expected it would get to be so big so fast.”
Rhyne says that while it can take up to 10 years to develop, test, and produce a vaccine, PPPs can speed up the process. For GSK’s Ebola vaccine candidate, the US National Institutes of Health, which includes NIAID, has facilitated Phase III clinical trials in Liberia – testing that would be challenging for the company to do on its own.
“The cooperation between public and private partners to accelerate the Ebola vaccine is an example of the best cooperation,” Rhyne says. “Through a broad range of partners, we have been able to accelerate discovery at a rapid pace.”
GSK says in addition to partnering with NIAID, it is relying on significant support from the World Health Organization, regulators, governments and others involved in the global response to help overcome a number of hurdles in the clinical development and manufacturing processes.
The company also says it has received funding from public and private entities to support Ebola research. In October the company was promised $3 million from the Gates Foundation to manufacture a second round of vaccines for testing if current trials prove successful. The Swiss government also gave $1.8 million and the European Commission contributed about $19 million to support the next phase of clinical testing.
GSK, for its part, says it has donated approximately $675,000 to support healthcare worker training, disease education and prevention efforts and about a million dollars worth of antibiotics. And last week, the pharmaceutical heavyweight sent an initial shipment of 300vials of the vaccine for the clinical trials in Liberia, where more than 3,500 people have died from Ebola.
The company says it has also begun manufacturing an additional 20,000 doses of the vaccine and claims it is “assessing all options to scale up production” and that it “supports stockpiling the vaccine for future outbreaks.”
The promise of partnership, but who benefits?
GSK is but one pharmaceutical company chasing an effective Ebola vaccine. NewLink Genetics and Merck Vaccines USA are currently working with the Canadian government on testing a product in human clinical trials. Other efforts led by Johnson & Johnson and Bavarian Nordic as well as by Novavax are also rushing to produce variants of an Ebola vaccine candidate.
It is too soon to know the cost of any vaccine for consumers, but GSK is considering a number of options to make it affordable in developing countries, collaborating with partners like the Gates Foundation and GAVI, says Rhyne.
Still, MSF’s Rius voiced concerns that the vaccine will be stockpiled and used to protect Americans and Europeans instead of Africans.
And many are questioning why the global community, especially pharmaceutical companies, waited so long to intervene in the first place.
“It’s a real shame and stain on the international community that it’s taking this long to come up with a vaccine,” says Phuoc Le, program director for global health hospital medicine at the University of California San Francisco who has spent significant time in Liberia training community health workers who are the first point of contact with Ebola patients.
“Now we’ve spent much more money on the crisis here than we ever would have had we nipped it in the bud if we had addressed it in April,” he says.
Lessons learned
Today, public fervor around Ebola has died down. Advocates worry that the waning media attention will leave West African countries even more vulnerable to future outbreaks, citing the decimated public health infrastructure, abandoned hospitals and doctors who died from Ebola themselves after treating sick patients.
Public awareness groups like ONE are promoting accountability by tracking public and private funds pledged and delivered to address Ebola. GAVI already has committed $300 million to buy Ebola vaccines.
“In the lead up to the [US midterm] elections, Ebola was one of the biggest issues,” says Erin Hohlfelder, ONE’s Global Health Policy Director. “How quickly we forget…We have to make sure this stays on the global agenda.”
With more than 8,500 deaths from Ebola, producing a viable vaccine is still a top priority for the public health community, one that will likely receive a boost thanks to the PRV subsidy made available through the new law.
The World Bank’s Kim emphasized this point at Tuesday’s Georgetown lecture. He said that greater incentives, like PRVs, to produce vaccines and drugs are part of adequately handling a public health crisis. Not partnering with the private sector, Kim warns, has been shown to have dire consequences.
Still, the WHO’s spokesperson Margaret Harris is cautious about the incremental progress PPPs have made thus far in the fight against Ebola, pointing out that porous borders compromise traditional means of containing an epidemic and disseminating vaccines.
“Infectious diseases don’t care who you are or where you are, they come and get you,” she says. When it comes to the consequences of ignoring resource poor countries lacking basic infrastructure, Ebola is a devastating lesson.
“When the crisis ends, we need to take stock… It’s a bit of a black eye on all of us,” ONE’s Hohlfelder says. “A problem there is a problem here. Nobody realized that until Ebola hit.”
Editor's Note: This is a follow-up piece to "Branding Health," a Special Report for GlobalPost published in September 2014 and produced by The GroundTruth Project. The multimedia series, which investigated the rising role of the private sector in global health, was supported in partnership with the Kaiser Family Foundation.
Correction: This article has been modified to reflect the correct spelling of the surname ONE's Global Health Policy Director. It is Hohlfelder, not Holderfelder.
Laura Rena Murray is a San Francisco-based investigative journalist covering public interest and accountability stories that highlight corruption, mismanagement and human rights violations. She has written for Al Jazeera America, New York Times, San Francisco Chronicle, SF Weekly, 100Reporters and the Center for Public Integrity. Her work has been recognized by the Overseas Press Club, Investigative Reporters and Editors, Daniel Pearl Investigative Journalism Initiative, the Nation Institute and the National Lesbian and Gay Journalism Association. @laurarenamurray
Every day, reporters and producers at The World are hard at work bringing you human-centered news from across the globe. But we can’t do it without you. We need your support to ensure we can continue this work for another year.
Make a gift today, and you’ll help us unlock a matching gift of $67,000!