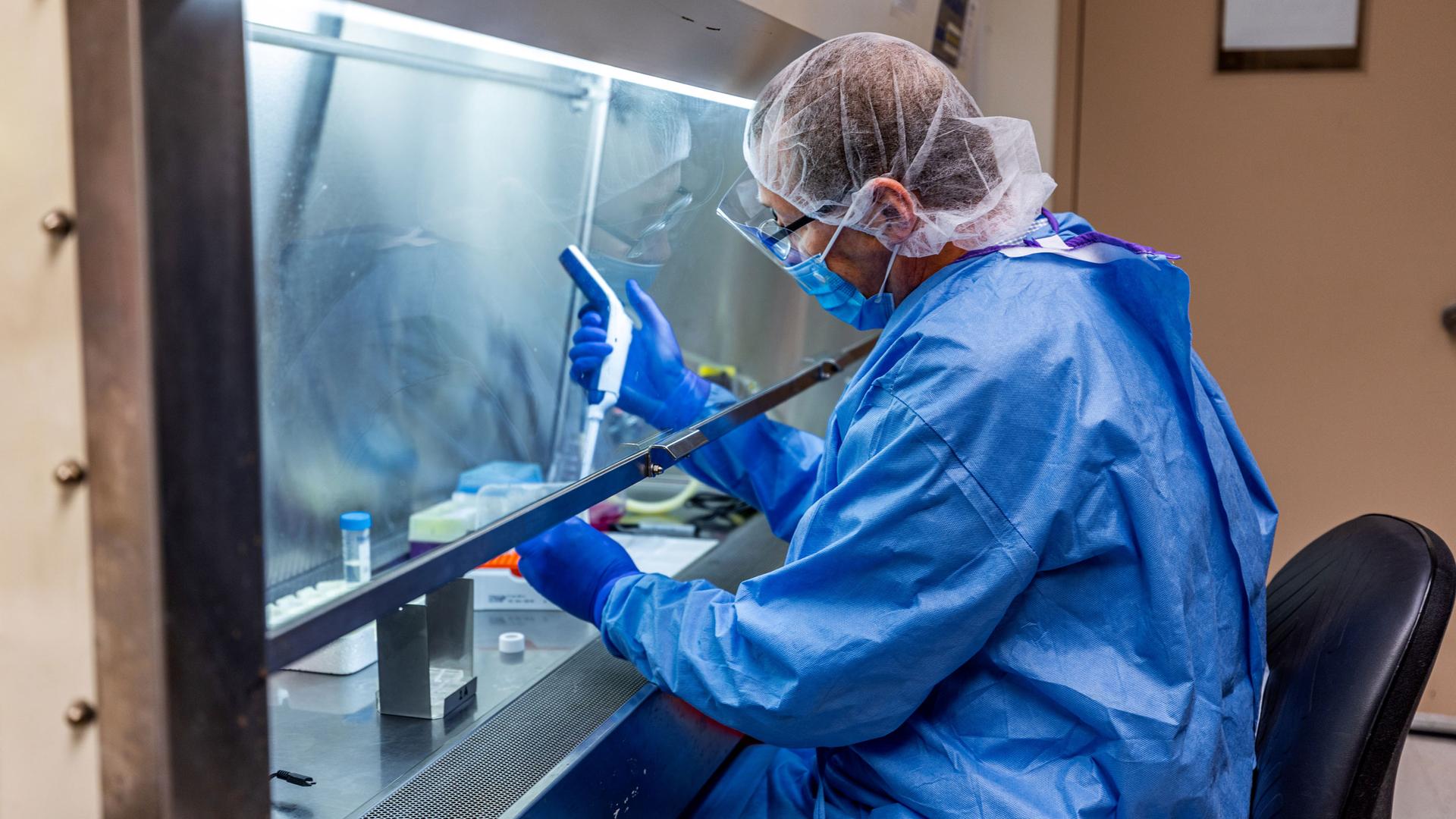
A researcher at the University of Pittsburgh works on a COVID-19 vaccine candidate, a fingertip-sized patch with dissolvable microscopic needles, in Pittsburgh, Pennsylvania, March 28, 2020.
The novel coronavirus pandemic has prompted a global race for treatments and vaccines.
But, when a treatment does become available, who gets access to it?
This question is of growing concern to policymakers and medical officials around the globe. Médecins Sans Frontières/Doctors Without Borders (MSF) has cautioned against patents and profiteering on treatments and tests for COVID-19, and urged governments to prepare to take measures like price controls “to ensure availability, reduce prices and save more lives.”
Related: COVID-19: The latest from The World
Dr. Manuel Martin is an adviser with Médecins Sans Frontières’ access campaign, based in Geneva. He spoke with The World’s Marco Werman and says a potential monopoly by one pharmaceutical company worries him.
“First, monopolies allow companies to set high prices, which are unaffordable for the most vulnerable. And this is not only amoral, but also dangerously stupid in the context of a pandemic, because we need as many people as possible to access vaccines if we’re going to defeat this thing and that’s just how herd immunity works,” Martin said. “And the second issue with monopolies is that they increase the risk of one country hoarding all of the supply of a treatment or vaccine, leaving very little for everybody else. And this is something we’ve seen before, actually, during the H1N1 pandemic of 2009, where high-income countries hogged all of the vaccine supply, crowding out low- and middle-income countries.”
Related: Is coronavirus reshuffling the global power deck?
Marco Werman: This pandemic with the coronavirus, it appears that there is a level of collaboration, though, for vaccine and drug research that the world has never really experienced. So, I mean, do you agree with that, first of all?
Dr. Manuel Martin: Yes. I mean, there’s organizations like CEPI, which stands for the Coalition for Epidemic Preparedness Innovations, which is leading the charge in a number of vaccine candidates. They have eight vaccine candidates in their pipeline. They were created, as a matter of fact, precisely because we didn’t have vaccines to treat emerging infections. And this was one of the lessons that we learned out of the 2014, 2016 Ebola outbreak.
We didn’t have any tools to fight this epidemic. And then learning from that lesson, in 2017, CEPI was created with large amounts of public and philanthropic monies to finance the research and development into these vaccines. Recently, they’ve been making some very encouraging steps when it comes to access and the sharing of the supply, which will come out of any CEPI-funded vaccine.
Related: As coronavirus spreads, poor communities in Kenya are left vulnerable
So, what is the access concern then about monopoly and big pharma that might stand in the way of treatment access? It doesn’t really sound like that’s a big problem.
Well, we don’t know that. CEPI is just one player. CEPI, as I mentioned, is funding eight vaccine candidates. But we know that there are currently 54 in the pipeline and we don’t know what the access will look like for the others. And even for CEPI-funded vaccines, we heard that the US had made a bid worth $1 billion for a vaccine candidate that was funded by CEPI for exclusive access. And it’s this kind of national control that we can’t accept and that is very dangerous. So, there’s work to be done by the international community to make sure that any vaccine that becomes available will be manufactured not just in one location, but in several locations across the world to match both the demand and also to dilute the risk of a nationalistic takeover.
Related: Gaza Strip fears spread of the coronavirus, Palestinian epidemiologist says
And how is that enforced?
So, we would really like to see the establishment of some kind of global coordinating mechanism that would distribute the initial vaccine supply based on public health needs, obviously prioritizing health care workers and the most vulnerable. This could be under the auspices of the WHO, for instance, but doesn’t necessarily have to be. A number of actors need to really come together and agree on a set of principles and practices to really make this happen.
This interview has been edited and condensed for clarity.